Human skin contains approximately 2 million sebaceous glands, with particularly high concentrations on the face (400-900 glands per cm²). These specialized organs reside in the dermis and play a crucial role in skin health by synthesizing and secreting sebum, a key component of the skin’s hydrolipidic film. Sebum serves multiple protective functions: it shields the skin from environmental damage and dehydration while maintaining the suppleness of both skin and hair.
Physiology of the sebaceous gland
The pilosebaceous compartment
Each sebaceous gland is associated with a hair follicle to form what’s called the pilosebaceous unit. Located in the dermis, the gland connects to the hair follicle through an excretory duct, creating a pathway for sebum to travel along the hair root and reach the skin surface (Figure 1).
 Figure 1: Schematic representation of sebocyte differentiation and sebum secretion within the sebaceous gland. Adapted from Sneider et al. Int J Biochem Cell Biol. 2010.
Figure 1: Schematic representation of sebocyte differentiation and sebum secretion within the sebaceous gland. Adapted from Sneider et al. Int J Biochem Cell Biol. 2010.
Sebocytes
Sebocytes are the specialized cells that make up most of the sebaceous gland and are responsible for the synthesis and secretion of sebum. The gland’s architecture is organized into three concentric zones, each representing a different stage in the sebocyte lifecycle (Figure 1):
- The Peripheral Zone (Germinative Layer): Around the gland’s outer edge lies a monolayer of undifferentiated, proliferative cells. These cells express stem cell markers including KRT15, TNC, KRT75, and FST, along with keratin 7, an early sebocyte marker. Characterized by their flattened shape and visible nucleus, these cells gradually enter a slow apoptotic process as they differentiate, accumulating lipids while migrating toward the gland’s center, into the maturation zone.
- The Maturation Zone: As sebocytes mature, they expand in volume and begin expressing specific markers of differentiation, such as Fatty Acid Desaturase 2 (FASD2) and Epidermal Membrane Antigen (EMA). Throughout this phase, they progressively start synthesizing sebum.
- The Necrosis Zone: Upon reaching full maturity, sebocytes release their sebum content through a holocrine process—a mechanism where the cell membrane ruptures. The released sebum then flows through the excretory duct to the skin surface.
Sebum composition and function
Composition of sebum
Sebum is a complex lipid mixture with a characteristic composition:
- Glycerides: 30-50%
- Fatty acids (including sapienic acid): 15-30%
- Wax esters: 26-30%
- Squalene: 12-20%
- Cholesterol: 1.5-2.5%
While many of these lipids are also found elsewhere in the body, squalene and wax esters are signature components of sebum.
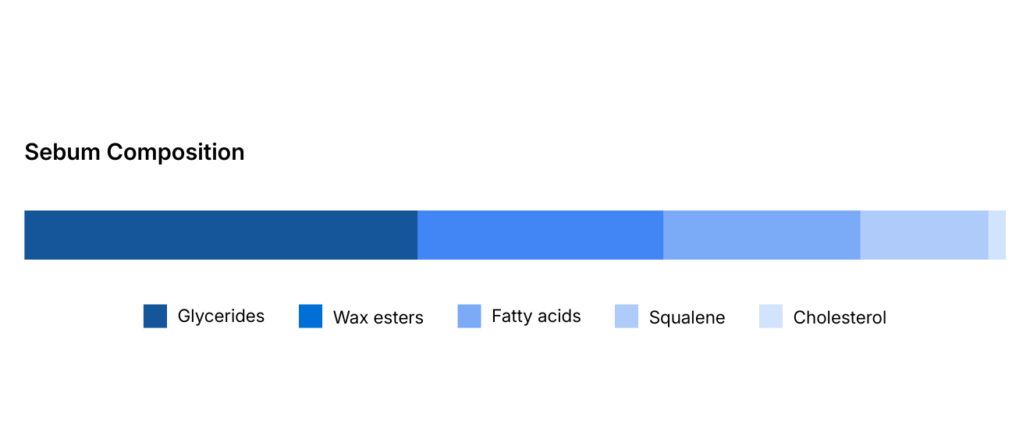
Figure 2: Composition of sebum
The biological functions of sebum
Beyond its primary function as a protective barrier preventing skin dehydration, sebum serves additional functions. It possesses antibacterial properties through the action of oleic and palmitoleic acids, while vitamin E and other substances provide antioxidant protection.
Sebum and skin and hair textures
The amount of sebum produced varies between individuals, directly influencing skin and hair characteristics. Insufficient sebum secretion results in dry skin or brittle hair, while excessive production (hyperseborrhea) leads to oily skin and greasy hair. In some cases, this overproduction can trigger skin conditions like acne.
Regulation of sebum production under normal conditions
Sebum production is a process controlled by various mechanisms.
Hormone regulation
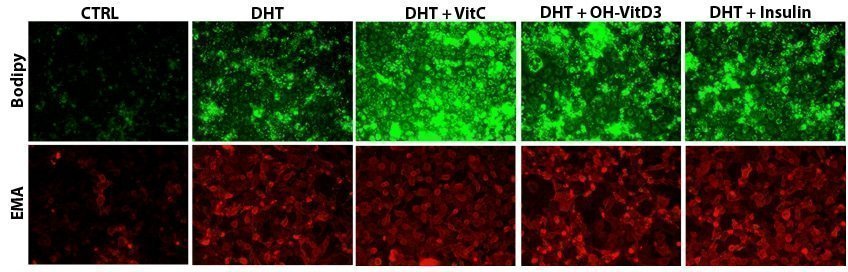
Sebum production by sebocytes is primarily regulated through hormonal signaling pathways. A central mechanism involves the enzyme 5-α-reductase, which converts testosterone into dihydrotestosterone (DHT), the principal androgen regulating sebaceous activity. DHT binds to androgen receptors (AR) within the sebocyte cytoplasm, initiating signaling cascades that stimulate lipid synthesis.
In addition to androgens, growth-related hormones also modulate sebaceous function via distinct mechanisms. Insulin, insulin-like growth factor (IGF), and hydrocortisone enhance sebum production by promoting sebocyte growth, differentiation, and proliferation.
Figure 3. Impact of dihydrotestosterone (DHT) and other lipogenic factors on lipid production (assessed by BODIPY staining) and on sebocyte differentiation (assessed by epithelial membrane antigen, EMA) in a human sebocyte model expressing androgen receptors.
Other regulatory factors
Several non-hormonal factors also shape lipid synthesis:
- Endogenous Factors: Lipogenic activity may respond to other non-hormonal endogenous lipogenic factors. Products of fatty acid metabolism, such as cholesterol and cholecalciferol (vitamin D), influence sebum production. Molecules of the retinoid family—including retinoic acid, retinol, and vitamin A—also play regulatory roles.
- Environmental: Exogenous factors affect both the quality and quantity of sebum secretion:
- Pollution: Whether from natural sources or human activities (ozone, industrial emissions, agricultural practices, cigarette smoke), pollution alters sebum composition and may stimulate its secretion.
- UV Exposure: Sun damage from ultraviolet radiation impacts the quality of sebum at the skin surface.
- Diet: Nutritional intake, particularly of specific fatty acids like cholesterol, appears to influence both the regulation and quality of secreted sebum.
Need to address hyperseborrhea to develop a new cosmetic product for oily and acne-prone skin?