Related Publications
SELECTED PUBLICATIONS ON ALOPECIA AREATA
Involvement of ILC1-like innate lymphocytes in human autoimmunity: lessons from alopecia areata
Mouse Models of Alopecia Areata: C3H/HeJ Mice Versus the Humanized AA Mouse Model
Hair follicle immune privilege and its collapse in alopecia areata
>> Check the full list HERE.
Conference Contributions
We share our research on dermatology and trichology through international conferences and publications, contributing to the advancement of research in these fields.
>> Check our past contributions HERE.
Preclinical Research Solutions for Alopecia Areata
IN VITRO MODELS
- Experimentally-induced AA-like phenotype in primary isolated ORSK (outer root sheath keratinocytes)
- Immune cells from healthy donors or AA patients
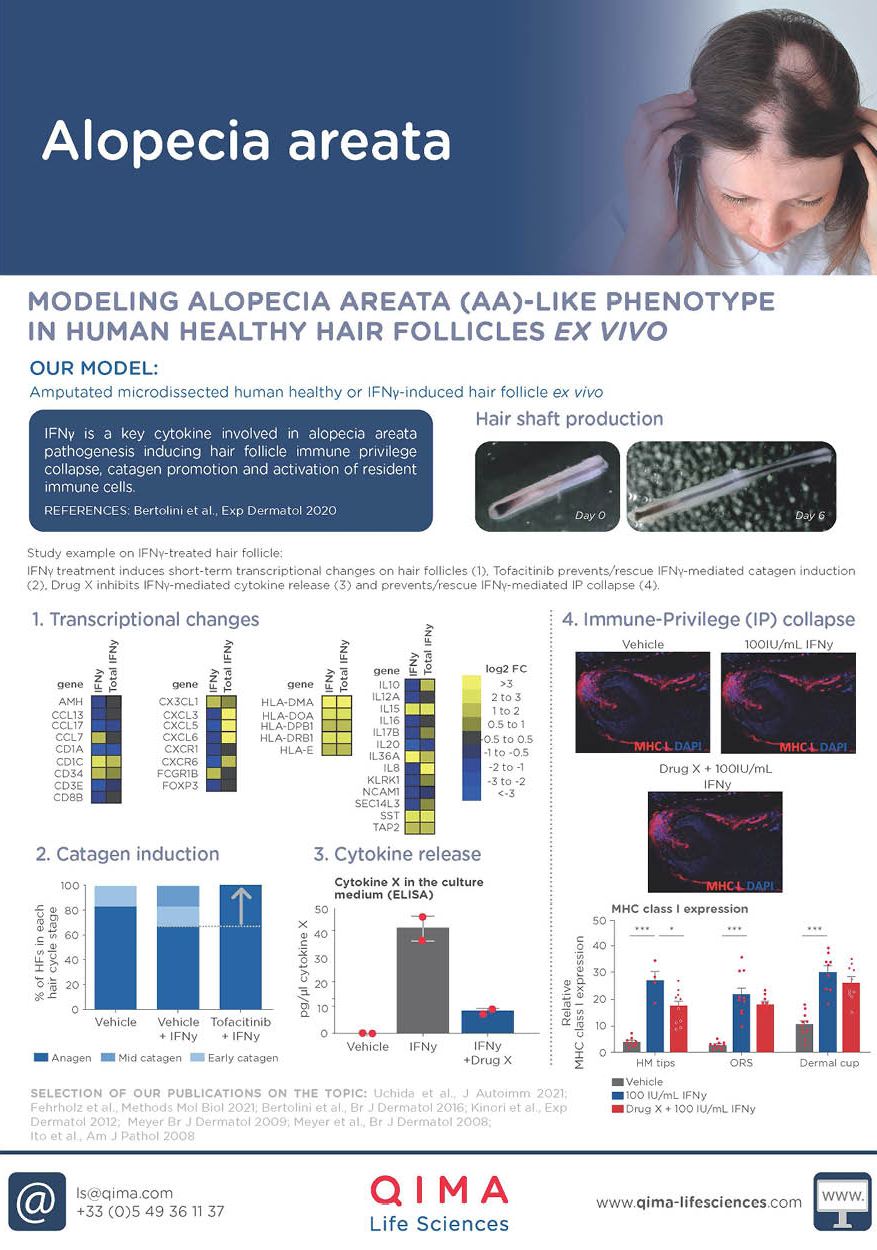
EX VIVO MODELS
- Human scalp skin explants
- Healthy or diseased human hair follicle organ culture
- Experimentally-induced hair follicle immune privilege collapse
- Co-culture of human hair follicles and human blood- or skin-derived immune cells
- Organ culture of lesional and non-lesional skin from AA patients
IN VIVO MODELS
- Humanized mouse model of AA (created through a collaboration with Prof. Amos Gilhar, Skin Research Laboratory, Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Haifa, Israel)
Clinical Research Solutions for Alopecia Areata
BIOANALYSIS OF CLINICAL SAMPLES
- Sample collection (scalp skin biopsies)
- Analysis and quantification of cellular components (proteins, lipids) via analytical chemistry
- AA biomarker analysis in tissue, blood and non-invasive collected samples
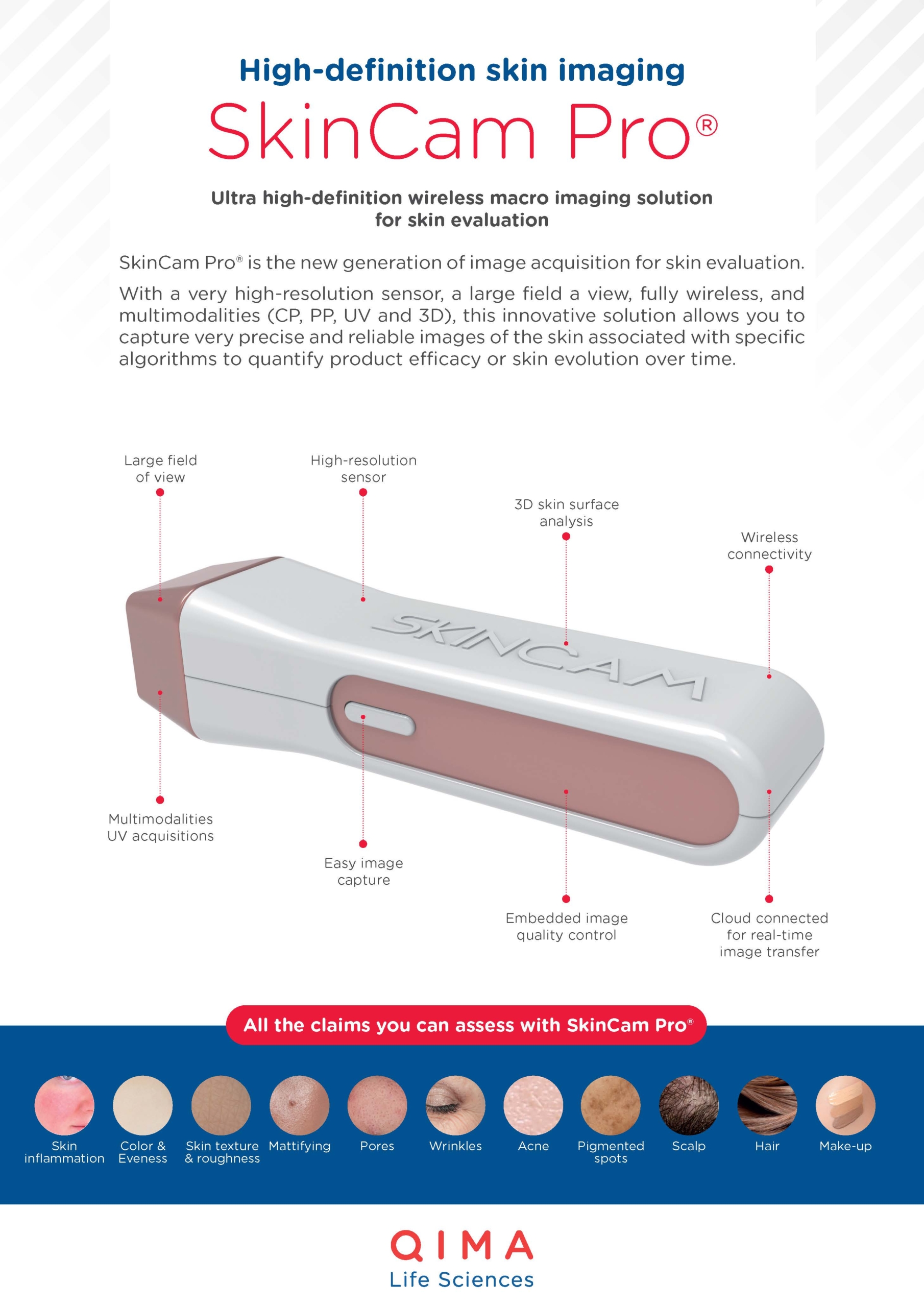
CLINICAL IMAGING
- Image capture
- Image analysis of AA lesions
CLINICAL TRIALS
- Clinical study implementation
- Clinical study performance
- Data management
- Data analysis
Alopecia Areata Study Examples
IFN-γ UPREGULATES IMMUNE PRIVILEGE MARKER EXPRESSION IN KERATINOCYTES IN VITRO
Test: Expression of MHC class I and -II
Method: Immunofluorescence staining
Model: Outer Root Sheath Keratinocytes (ORSK) in vitro
Interpretation of results: Stimulation with IFN-γ induces the expression of the immune privilege markers MHC class I and II in ORSK.
TOFACITINIB PREVENTS IFN-γ INDUCED PREMATURE CATAGEN INDUCTION IN HEALTHY HUMAN HAIR FOLLICLES EX VIVO
Test: Microscopic analysis of hair cycle stages
Method: Quantitative (immuno-)histomorphometry
Model: Healthy human hair follicle organ culture ex vivo
Interpretation of results: Stimulation with IFN-γ induces premature catagen development, a hallmark of AA, which is prevented by addition of the JAK inhibitor Tofacitinib.
LESIONAL AA SCALP SKIN IS CHARACTERIZD BY HIGHER NUMBERS OF CD3+ T CELLS
Method: Immunofluorescence staining
Model: Non-lesional and lesional AA scalp skin organ culture ex vivo
Interpretation of results: The number of peri- and intrafollicular CD3+ T cells is significantly higher in lesional compared to non-lesional scalp skin, indicating an ongoing inflammatory response.
HAIR RE-GROWTH IS INDUCED BY DEXAMETHASONE AND MINOXIDIL IN THE HUMANIZED MOUSE MODEL OF AA
Test: Macroscopic analysis of hair re-growth
Method: Quantification of the number of hairs/graft
Model: Humanized mouse model of AA
Interpretation of results: Treatment of human, AA-induced scalp skin xenografted on SCID mice with a combination of Dexamethasone and Minoxidil efficiently induces hair re-growth.


At QIMA Life Sciences, we are committed to staying at the forefront of dermatology research by developing innovative approaches.
We offer smart solutions for studying alopecia areata using validated models at both preclinical and clinical stages, making us the perfect partner for your research.
Explore Our Models & Assays in Our Flyer
Interested in Learning More?
Explore Other Related Topics
SKIN & HAIR RESEARCH
HIGH-DEFINITION IMAGING: SKINCAM PRO®