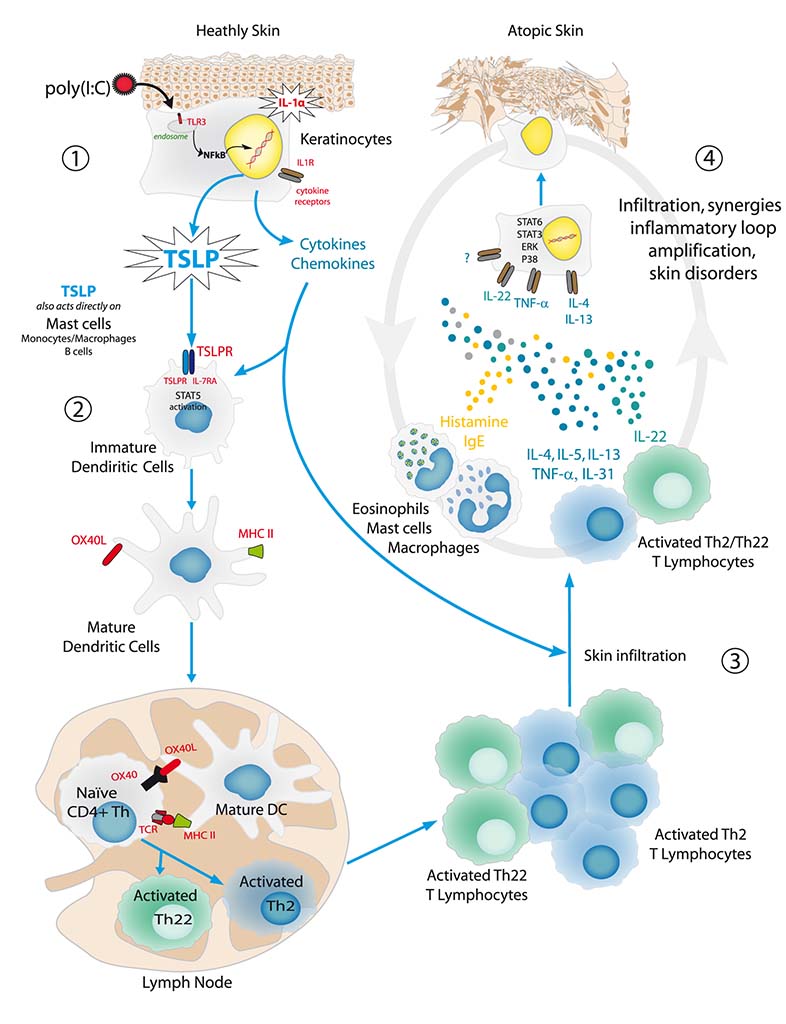
Atopic dermatitis – immune response and skin lesions
TH2/TH22 immune response and other agents of atopic dermatitis
The Th2 and Th22 TL migrate to the lesion area, where they release type Th2 (IL-4, IL-5, IL-13, IL-31, TNF-α) and Th22 (IL-22) cytokines respectively [Test : PBMC-0009]. These Th2/Th22 cytokines have different functions in the immunity response:
- IL-4 maintains the CD4+ TL differentiation in TL of type Th2/Th22 as well as the massive secretion of IgE by plasma cells. These secreted IgE bind to the FcεRI receptors located on the mast cells, basophil cells and macrophage cells, thus sensitizing them to the allergen.
- TNF-α activates various types of infiltrating cells, such as monocytes and macrophage cells. Moreover, it stimulates the secretion of various chemokines and innate immunity molecules by the keratinocyte.
- IL-22 significantly modulates the keratinocyte metabolism, which results in abnormal epidermal differentiation.
In conjunction with these inflammatory cytokines, the sensory neurons secrete neuropeptides (CGRP and substance P) [Tests : NS-0004; NSNB-0001] that stimulate various cell populations (mast cells, T lymphocytes, plasma cells and eosinophil cells) and contribute to vasodilation and itching.
Atopic dermatitis: keratinocyte response, inflammatory loop and chronicity
The binding of Th2/Th22 cytokines with their receptors on the keratinocyte will activate the signaling pathways, thus generating synergic responses in terms of gene expression [Tests : NHEK-0038; EPIBA-0071], modification of metabolism and keratinocyte structure. Notably :
- IL-4 and IL-13 mainly stimulate the STAT6 signaling pathway.
- IL-22 and IL-31 mainly activate the STAT3 protein phosphorylation.
- TNF-α induces an NFκB nuclear translocation [Test : NHEK-0015].
These cytokines also stimulate, more or less selectively, the MAP kinase pathway (p38, ERK, etc.).
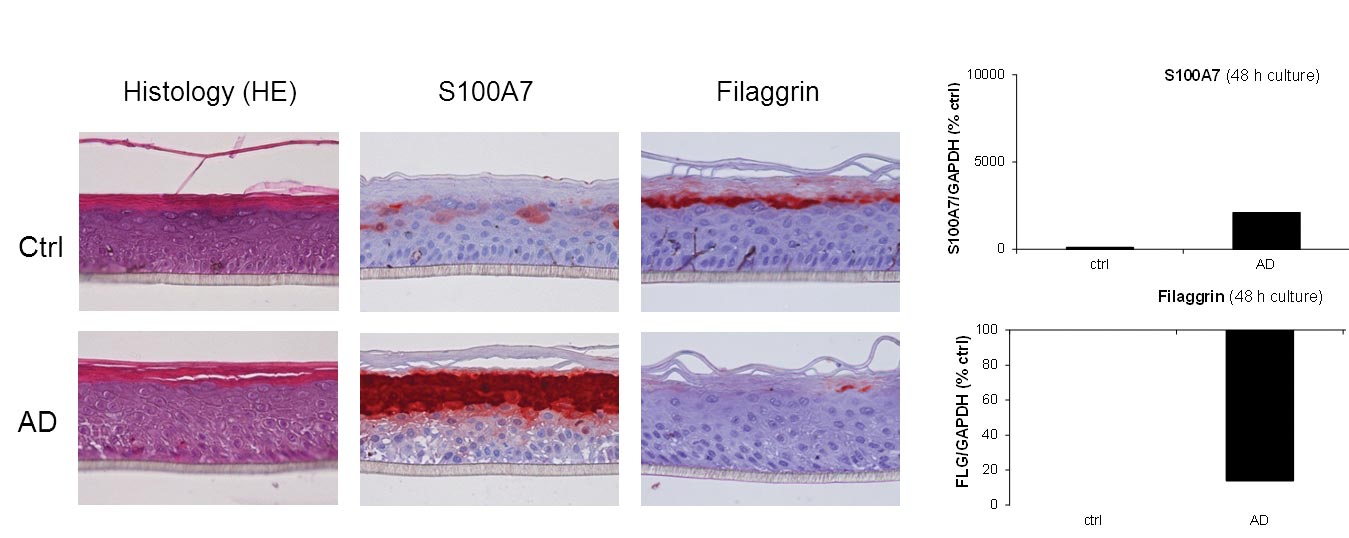
The activation of these signaling pathways disturbs the keratinocyte metabolism (e.g. apoptosis) and stimulates the production of chemokines leading to the amplification of an inflammatory loop and to pathology chronicity. This stimulation also considerably modifies the skin structure, mainly by suppressing the epidermal constituents involved in its terminal differentiation (filaggrin, etc.) [Test : EPIBA-0073] and finally results in skin lesions that are characteristic of atopic dermatitis. In addition, atopic dermatitis is characterized by a poor production of antimicrobial defense molecules, especially β-defensine and by skin superinfections.
References
- Cho, SH., et al. (2001). J Invest Dermatol. 116:269-274.
- Odhiambo, JA., et al. (2009). J Allergy Clin Immunol. 124(6):1251-1258.
- Oyoshi, MK., et al. (2009). Adv Immunol. 102:135-226.
- Spergel, JM., et al. (2010). Ann Allergy Asthma Immunol. 105:99-106.
- Schlievert, PM., et al. (2010). J Allergy Clin Immunol 125:39-49.
- Boguniewicz, M., et al. (2010). J Allergy Clin Immunol. 125:4-13.
- Palmer, CN., et al. (2006). Nat Genet. 38:441-6.
- Kinoshita, H. et al. (2009). J Allergy Clin Immunol. 123:179-86.
- Anh, T. et al. (2011). J Invest Dermatol. 131:2205-2212.
Related posts
Check out Bioalternatives’ updates and experience new testing ideas
- New assays, models and services
- Posts and publications
- Events