Atopic dermatitis: Physiopathology and clinical signs
Epidemiology
Atopic dermatitis is the most common dermatosis affecting children: 65% of the patients are less than a year old and 85% are below 5 years. The prevalence of this pathology is constantly on the rise and currently affects 10 to 25% of the population. This increase is related to the lifestyle in industrialized countries, where 20% of the children suffer from this dermatosis.
Clinical signs of atopic dermatitis
The symptoms of atopic dermatitis mainly appear on the skin. Pruritus, an intense itching resulting from xerosis (skin dryness) and histamine release, is the main symptom of this pathology [Tests: MAST-0001; BLOO-0008]. Following this itching, excoriations appear on the skin and form lichenification patches (skin thickening). These skin lesions are accompanied by the formation of oozing scabs as well as erythema and papules. Moreover, in contrast with psoriasis, cutaneous keratinocytes in atopic dermatitis patients express few antimicrobial defense molecules (β-defensin) [Tests : NHEK-0035; NHEK-0037]. This explains why this dermatosis often occurs with complications, among which the most common are bacterial or viral superinfections. For example, Staphylococcus aureus, which is often found in skin superinfections [Test : EPIBA-0060], exacerbates skin inflammation by secreting toxins and may cause impetigo.
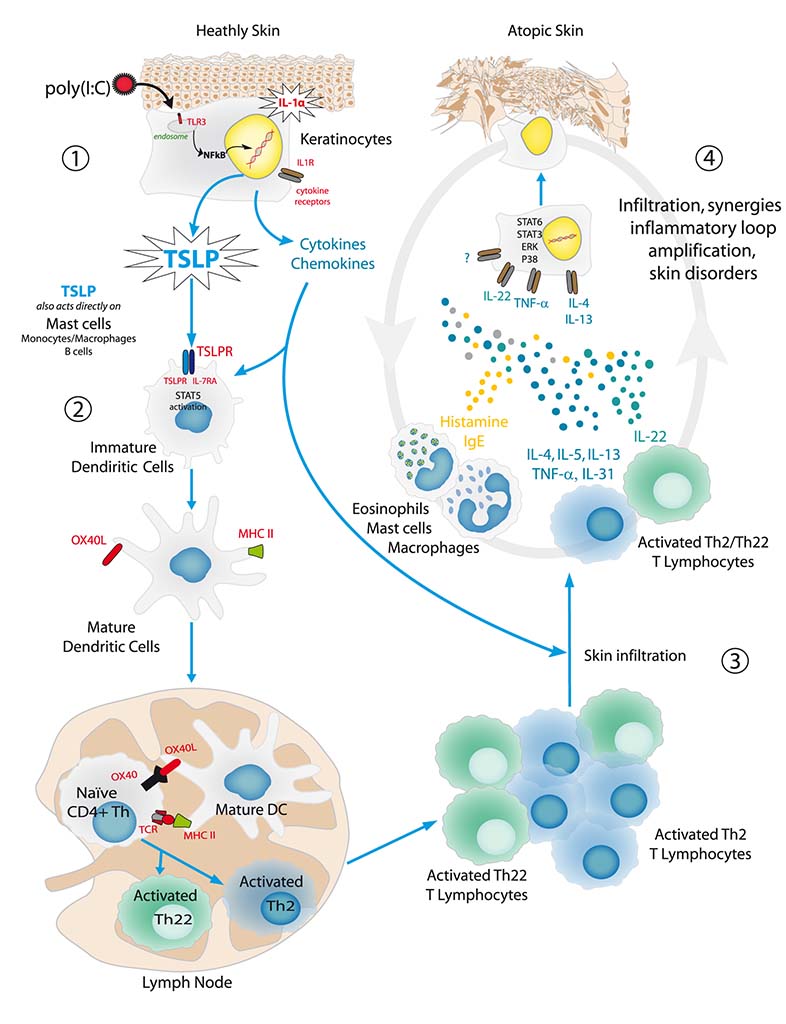
Physiopathology of atopic dermatitis
The cause of atopic dermatitis is often linked to an epidermal barrier dysfunction, generally due to a mutation in the filaggrin gene. This structural anomaly facilitates skin lesions and leads to increased skin permeability, promoting the entry of antigens. Barrier dysfunction and antigen entry are at the root of the sensitization stage of atopic dermatitis. It is in a second stage, called the effector stage, that the appearance of pathological symptoms is noticed. This stage may be divided into several steps: initiation, activation of dendritic cells, polarization of Th2/Th22 lymphocytes as well as activation of other agents of AD (mast cells, etc.) and finally, an inflammatory loop between the keratinocyte and the infiltrating cells, leading to pathological skin.
Check out Bioalternatives’ updates and experience new testing ideas
- New assays, models and services
- Posts and publications
- Events